You can never have enough good explanations and descriptions of what neuropathy is (especially for people new to the condition) and today's post from www.symptomfind.com (see link below) is a very useful general information article. Clear and easy to understand information will always be valued by this blog and for that reason this article is worth a read for everybody coming in contact with neuropathy.

By Tina M. St. John, MD Medically Reviewed:Tom Iarocci, MD Published:May 15, 2014
Neuropathies are a diverse group of chronic nerve conditions that may cause painful cramps, loss of muscle and the odd sensations of pins and needles.
You know the feeling. You cross your legs or sit back on your heels for too long and they fall asleep. The numbness, tingling and pain you briefly feel are nearly identical to some of the symptoms people with peripheral neuropathy might experience.
Peripheral neuropathy, often referred to as neuropathy or nerve damage, is a catch-all term that encompasses a broad group of medical conditions involving damage or malfunction of one or more peripheral nerves.
What Are the Peripheral Nerves?
Your peripheral nerves are those outside your brain and spinal cord, and they form a complex signaling network that carries messages between your body and brain. They help your brain manage many functions, from movement to breathing.
There are three kinds of peripheral nerves: sensory, motor and autonomic.
Sensory Nerves affect how well you detect sensations, such as pain, heat, cold or touch. For example, they are what tell your brain that a pot of boiling water is hot.
Motor Nerves control your muscles and movement. Say your nose itches. Messages from your brain tell your body to scratch your nose, and those actions are carried out instantly by your motor nerves.
Autonomic Nerves control the automatic functions of your internal organs and body systems, such as digestion, heart rate and blood pressure.
Peripheral neuropathy can affect either one, a few or many nerves. In fact, many types of neuropathy involve damage to both the sensory and motor nerves.
Symptoms of Neuropathy
There are more than 100 types of peripheral neuropathy, and the primary functions of the damaged nerves determine what symptoms you experience. Symptoms can develop suddenly and progress quickly or, more commonly, evolve gradually.
Sensory Nerve Damage:
Tingling or prickling sensations, which often develop first;
Burning sensations; and
Loss of sensitivity to touch and temperature.
Motor Nerve Damage
Muscle weakness, which may occur suddenly or gradually;
Muscle cramps;
Muscle twitching; and
Difficulty moving body parts, such as your arms or legs. Running, walking and other tasks like carrying groceries or turning a doorknob become challenging
Autonomic Nerve Damage
Feeling full long after a meal;
Diarrhea or chronic constipation;
Sweating more or less than usual;
Dizziness when you stand up;
Cool feet and hands;
Difficulty emptying your bladder; and
Erectile dysfunction
The specific symptoms you experience, the timing of them and their location all help your doctor determine the type of peripheral neuropathy you have and possible causes.
Causes of Peripheral Neuropathy
There are many possible causes of neuropathy, from sports injuries to certain conditions or diseases. Two of the biggest risk factors include diabetes and alcoholism. The different neuropathy causes are grouped into broader categories:
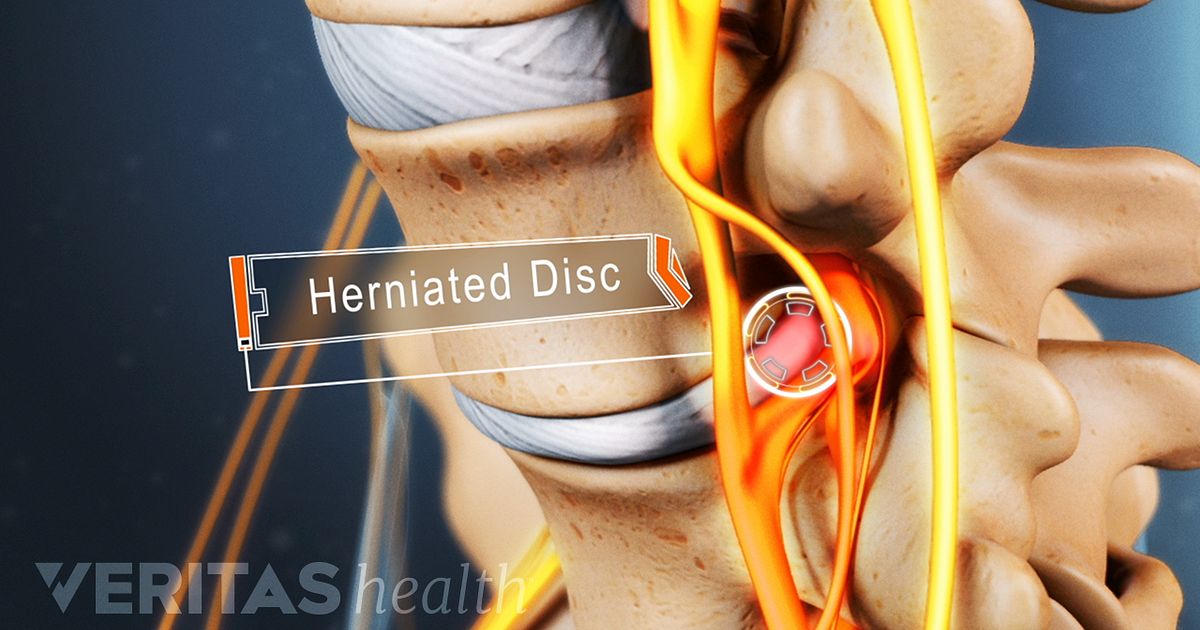
Nerve compression or injury, such as,
Carpal tunnel syndrome
Thoracic outlet syndrome
Infection-related causes, such as:
HIV/AIDS
Lyme disease
Hepatitis B and C
Shingles (herpes zoster)
Guillain-Barré syndrome
Immune system disorders, such as:
Systemic lupus erythematosus
Rheumatoid arthritis
Celiac disease
Cancerous conditions, such as:
Multiple myeloma
Lymphoma
Paraneoplastic syndrome
Systemic or metabolic diseases, such as:
Diabetes
Kidney failure
Hypothyroidism
Inherited disorders, such as:
Charcot-Marie-Tooth disease
Toxins, such as:
Alcohol
Inhaled intoxicants (e.g., glue)
Heavy metals (e.g., lead, arsenic, mercury)
Organophosphate pesticides
Drugs and medications, such as:
Some chemotherapy drugs
Some HIV medications
Some heart and/or cholesterol medicines
Some psychiatric medications
Some antibiotics
Heroin
Nutritional deficiencies, such as:
Vitamin B12
Vitamin B6
Diagnosis and Treatment
Diagnosing the cause of peripheral neuropathy can be challenging. The location of your symptoms is one of the first things your doctor will consider if you’re being evaluated for neuropathy. Your doctor will begin by taking your medical history including what symptoms you’re experiencing, where and when they began, any ongoing medical conditions you have, and all medications or supplements you take. A thorough physical examination — which involves testing your reflexes, muscle strength, coordination and sensitivity to touch — is the next step.
To help narrow the list of possible causes, blood tests are often used to check for abnormalities. Your doctor may recommend electrodiagnostic tests, such as a nerve conduction study or an electromyogram (EMG), to determine how well specific nerves are functioning. Other tests, such as imaging studies, may be needed. Your doctor may refer you to a neurologist if the diagnosis is unclear or your symptoms are severe. Treatment for peripheral neuropathy depends on the cause but often involves strategies to both manage the underlying cause and relieve your symptoms.
Next Steps
For Patients
If you are feeling any new or persistent nerve-related symptoms, see your doctor, even if the symptoms come and go. Additionally:
Report all medications, herbs and supplements you take to your doctor. People commonly omit this information, but this information is important when determining the cause of peripheral neuropathy.
Don’t stop taking any prescribed medication without first checking with your doctor, even if you feel that medication might be the cause of your symptoms.
Seek immediate medical care if you experience sudden muscle weakness or have any difficulty breathing.
For Family Caregivers
If you suspect a loved one might have neuropathy, be vigilant if or when symptoms arise in your loved one. Be sure to:
Schedule a doctor’s appointment as soon as you notice symptoms.
Keep careful notes before and during the medical appointment to help the doctor determine how many nerves (or nerve groups) may be involved.
sources
Azhary H., MD, Farooq M., MD, Bhanushali M., MD, et al. “Peripheral Neuropathy: Differential Diagnosis and Management.” American Family Physician. 2010; 81 (7); pages 887-92. http://www.aafp.org/afp/2010/0401/p887.html. Accessed May 2014.
Shields R., Jr., MD. Cleveland Clinic. “Peripheral Neuropathy.” http://www.clevelandclinicmeded.com/medicalpubs/diseasemanagement/neurology/peripheral-neuropathy/. Accessed May 2014.
Patient.Co.UK. “Polyneuropathies.” http://www.patient.co.uk/doctor/Polyneuropathies.htm. Accessed May 2014.
World Federation of Neurology. “Peripheral Neuropathies.” http://www.wfneurology.org/cache/downloads/abspzqgpdgws0gkokg8kgsk84/Munsat_chapter7.pdf. Accessed May 2014.
Patient.Co.UK. “Mononeuropathies.” http://www.patient.co.uk/doctor/Mononeuropathies.htm. Accessed May 2014.
Rowland L., MD, Pedley T., MD. “Merritt's Neurology,” 12th Edition. Lippincott Williams & Wilkins 2010. Accessed May 2014.
http://www.symptomfind.com/diseases-conditions/peripheral-neuropathy-symptoms-causes-and-treatments/
.jpg)




 And the whey ..... dripped down overnight from the greek yogurt I found at the store. Kiva recommends Piima cheese but I couldn't find any. From two containers of the "Fage" I rendered one cup of whey.
And the whey ..... dripped down overnight from the greek yogurt I found at the store. Kiva recommends Piima cheese but I couldn't find any. From two containers of the "Fage" I rendered one cup of whey. In in goes..... with the honey and sugar and a little fizzy blessing.
In in goes..... with the honey and sugar and a little fizzy blessing. And while we wait we can stuff our faces with this creamy cheese leftover! It's perfect on cornbread.
And while we wait we can stuff our faces with this creamy cheese leftover! It's perfect on cornbread. Hope it works!
Hope it works!