Today's post from cidpneuropathysupport.com (see link below) looks at the role of Vitamin B in both the prevention of and treatment of neuropathy. This article looks at it from the inflammatory neuropathy angle but it can be argued that all neuropathy is inflammatory by nature. The nerves become inflamed and/or damaged through inflammation and a vitamin B deficiency is often seen as contributing to that. That said, you need to be tested by your doctor to establish a deficiency before embarking on vast amounts of supplements. For neuropathy patients with a normal Vitamin B level, there'll be enough extra in your daily multivitamin. There are also different forms of vitamin B and excessive amounts can bring about side-effects - best discuss it with your doctor.

Author: Shiraz Abbas May 27, 2017
Studies are now suggesting that vitamin B may have an important role in healing or easing the pain of peripheral neuropathy and CIDP type of neuropathy in particular.
Peripheral neuropathy is a disorder of the peripheral nerves. It is often characterized by weakness of limbs, numbness and pain. CIDP type neuropathy is a form of neuropathy in which there is a progressive and gradual destruction of the nerves through inflammation.
The vitamin B family of vitamins (also known as B complex vitamins) are critical for the proper functioning of the human body. They play a role in our immune system, energy, and red blood cell formation. Vitamin B12 is particularly important for neurological health and is a vitamin of choice to help treat neuropathy.
Vitamin B is commonly used to treat neuropathy. According to one study, people given high doses of vitamin B for four weeks had their pain reduced and saw improvement in their vibration perception threshold (VPT), that is, a testing that is used to measure large nerve fiber function in the body. People with lesser doses in a 8 week span saw lesser improvement.
Deficiency in B vitamins may lead to neurological problems. B12 in particular is important for the development of the central and peripheral nervous system. It has a critical role in maintaining the myelin sheath which ensures the transmission of nerve signals in the central and peripheral nervous system.
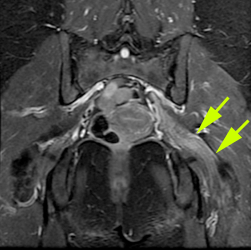
In neuropathy, especially CIDP type neuropathy, the signals between the spinal cord and other parts of the body are disrupted. With CIDP in particular, the myelin sheath is gradually but progressively damaged through inflammation and hence leading to an impairment of the transmission of nerve signals. This process of demyelination leads to axonal destruction. The disease is thus characterized by the following symptoms: weakness of the limbs, numbness, tingling sensation and pain. Loss of sensation and activity also happens depending on where the damage is occurring.
As B vitamins, particularly vitamin B12 play a role in maintaining a healthy peripheral nervous system, the vitamin may also play a role in the reconstruction of the nerves and more particularly the myelin sheath and hence helping the reduction of pain and improving sensation.
Some people with neuropathy may not be able to absorb vitamin B12 due to the loss of the “intrinsic factor” that is produced in the stomach and hence the loss of ability to absorb B12 through the digestive tract. In these cases like these, B12 may be injected into the body. Please check with your doctor if you have digestion problems with it comes to B12.
For those who can absorb it through the digestive tract, the following foods are high in B12 in addition to B12 supplements:
Beef Liver (71 mcg for a three-ounce serving, provides 2951% of the daily recommended intake).
Mackerel (16 mcg for a three-ounce serving, provides 661% of the daily recommended intake).
Sardines (8 mcg for a three-ounce serving, provides 333% of the daily recommended intake).
Read Meat (5 mcg for a three-ounce serving, provides 208% of the daily recommended intake).
Salmon (4 mcg for a three-ounce serving, provides 167% of the daily recommended intake).
Shiraz Abbas is the founder and manager of the CIDP Neuropathy Support Group. He is also one of the main community educators of IVIG therapy. He resides in Fresno, California. Shiraz can be contacted through our free CIDP advice service at 1-855-782-0574.
http://cidpneuropathysupport.com/cidp-neuropathy-and-vitamin-b/